Introduction to Ozempic and Similar Weight Loss Drugs
Ozempic and its counterparts are a class of medications primarily used for the management of type 2 diabetes and weight reduction. These drugs, known generically as semaglutide, function as glucagon-like peptide-1 (GLP-1) receptor agonists. GLP-1 is a hormone that enhances the secretion of insulin while simultaneously inhibiting the release of glucagon, leading to better blood sugar control. By mimicking this hormone, Ozempic facilitates improved glycemic regulation and contributes to significant weight loss.
The mechanism behind these medications involves several physiological processes. Firstly, GLP-1 receptor agonists delay gastric emptying, which helps to control appetite and reduce food intake. Additionally, they enhance insulin secretion in response to meals and decrease hepatic glucose production, leading to improved overall metabolic functioning. The efficacy of these agents in managing diabetes and promoting weight loss has been substantiated by numerous clinical trials and real-world evidence.
While the primary application of Ozempic and similar drugs is to aid individuals with type 2 diabetes, their benefits extend beyond glucose management and weight control. Emerging research suggests that these medications may also confer neuroprotective effects, potentially reducing the risk of developing neurodegenerative conditions such as Alzheimer's disease. This potential for neuroprotection has sparked considerable interest within the scientific and medical communities, propelling further investigations into the multifaceted benefits of GLP-1 receptor agonists.
The intrigue surrounding Ozempic and its alternatives lies not only in their immediate therapeutic applications but also in their broader implications for long-term health. As understanding deepens, these drugs could potentially reshape treatment paradigms for various conditions, heralding new avenues for disease prevention and management. This burgeoning field of research underscores the importance of continuing to explore and elucidate the diverse potentials of GLP-1 receptor agonists.
The Science Behind Neuroprotection and Alzheimer's Disease
Alzheimer's disease is a progressive neurodegenerative disorder characterized by cognitive decline, memory loss, and changes in behavior. It is the most common form of dementia, affecting millions worldwide, with significant emotional and economic impacts on patients, families, and healthcare systems. The pathology of Alzheimer's involves complex biological and neurological mechanisms that result in the deterioration of brain function.
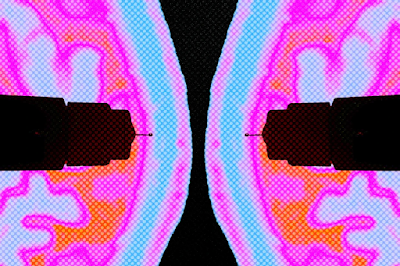
At the core of Alzheimer's disease are two hallmark features: amyloid plaques and tau neurofibrillary tangles. Amyloid plaques are extracellular deposits primarily composed of beta-amyloid peptides, while tau tangles are intracellular accumulations of hyperphosphorylated tau protein. These abnormal protein aggregates disrupt neuronal communication, leading to synaptic loss and neuronal death.
The formation of amyloid plaques involves the enzymatic cleavage of amyloid precursor protein (APP) by beta-secretase and gamma-secretase, producing insoluble beta-amyloid fragments that clump together. Simultaneously, tau protein, which normally stabilizes microtubules in neurons, becomes hyperphosphorylated and forms tangles that obstruct nutrient transport within cells. Collectively, these processes contribute to the progressive decline observed in Alzheimer's patients.
Neuroprotection refers to strategies or agents that prevent or slow the degeneration of neurons. For a drug to be considered neuroprotective, it must demonstrate efficacy in preserving neuronal health, promoting cell survival, or enhancing cognitive function in the face of disease-related insults. Criteria include reducing oxidative stress, inhibiting inflammatory pathways, and preventing toxic protein aggregation.
Recent research suggests that weight loss drugs like Ozempic may have neuroprotective effects. Ozempic, primarily used to manage type 2 diabetes and aid weight loss, mimics the hormone GLP-1, which influences glucose metabolism. Emerging studies indicate that GLP-1 analogs can cross the blood-brain barrier and may reduce amyloid and tau pathologies, decrease inflammation, and enhance neuronal survival, thereby fitting into the neuroprotective category. These findings open new avenues for therapeutic interventions targeting Alzheimer's disease.
Evidence Linking Ozempic-like Drugs to Alzheimer's Protection
Recent research has shed light on the potential benefits of Ozempic-like drugs, specifically for Alzheimer’s disease. Various preclinical and clinical trials have begun to explore the relationship between these drugs and neuroprotection. Importantly, findings indicate that these medications might offer protective effects against the neurodegenerative processes associated with Alzheimer’s.
Several preclinical studies have highlighted the potential mechanisms through which Ozempic-like drugs, often used for weight loss and diabetes management, may contribute to brain health. For example, these medications are believed to enhance neuronal survival, reduce inflammation, and promote neuroplasticity. Additionally, animal models have shown that treatments with these drugs can lead to a reduction in amyloid-beta plaques and tau tangles, both of which are hallmark features of Alzheimer’s pathology.
Clinical trials corroborate some of these findings, indicating that individuals receiving Ozempic-like treatments might exhibit slower cognitive decline compared to those not receiving such interventions. While these trials are in early stages, preliminary results are promising, suggesting potential neuroprotective effects. The exact mechanisms underlying these benefits are not entirely understood, but hypotheses include improved insulin signaling within the brain and reduced oxidative stress, both crucial factors in Alzheimer’s prevention.
Despite these encouraging findings, it is important to note the limitations of current research. Many of the existing studies are preliminary and involve small sample sizes, leading to challenges in generalizing the results. Furthermore, the long-term impacts of these drugs on brain health remain largely unknown, necessitating further investigation. Areas where more evidence is needed include large-scale longitudinal studies to confirm the effectiveness and safety of these medications for Alzheimer’s prevention.
Overall, while preliminary research is promising, the scientific community must continue rigorous investigation to fully understand the potential neuroprotective effects of Ozempic-like drugs. This will ensure that their application in clinical settings is both safe and beneficial for individuals at risk of Alzheimer's disease.
As the promising findings surrounding Ozempic-like weight loss drugs continue to unfold, their implications for Alzheimer's research and treatment regimens merit thorough examination. These drugs, primarily known for their efficacy in managing diabetes and aiding weight loss, now present a potential new frontier in neuroprotection. Integrating these medications into treatment plans for individuals at risk of Alzheimer's could represent a paradigm shift in how we address neurodegenerative diseases.
Integration into Treatment Plans
The integration of Ozempic-like drugs into existing Alzheimer's treatment regimens would necessitate a multi-faceted approach. Clinicians would need to balance the primary benefits of these medications with their newly discovered neuroprotective properties. This would involve careful patient selection, extensive monitoring, and possibly even the development of new protocols for dual-purposed treatments. Such an approach could delay disease onset or slow progression, offering a novel strategy beyond the current symptomatic treatment offerings.
Ethical Considerations
While the potential benefits are significant, ethical considerations must not be overlooked. The use of weight loss drugs for neuroprotection raises questions about long-term safety, accessibility, and the potential for off-label use. Ensuring that these drugs are prescribed responsibly and equitably will be paramount. Regulatory bodies will need to establish clear guidelines to steer this new application, balancing innovation with patient safety.
Future Research and Funding
Given the promising nature of these preliminary findings, future research will be pivotal. Funding initiatives aimed at understanding the mechanistic link between these drugs and neuroprotection will provide deeper insights. Longitudinal studies, clinical trials, and collaborative research across disciplines could lay the groundwork for new drug development tailored specifically for Alzheimer's prevention and treatment. Additionally, exploring the genetic and molecular pathways involved may uncover secondary benefits and further applications of these drugs.
The possibility of developing new medications inspired by the neuroprotective properties of Ozempic-like drugs opens up a new vista in Alzheimer's research. With continued investigation and responsible implementation, the intersection of metabolic health and neuroprotection could herald a new era in the fight against Alzheimer's disease.

.png)
Post a Comment